
Walk the lakes, forests 😀💚 Co.Cavan🇮🇪




·
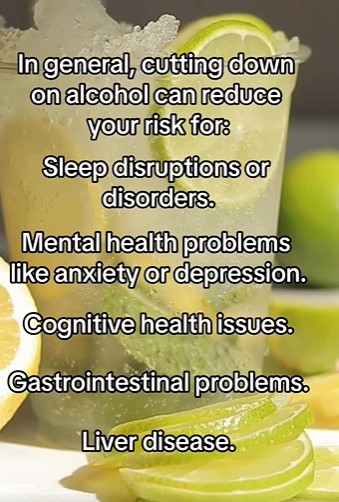
There are many health benefits related to abstaining from alcohol. If you’re looking to cut back or stop drinking altogether, here are 11 tips that can help. #HarvardHealth
Are you concerned about your alcohol intake? Maybe you feel that you’re drinking too much or too often. Perhaps it’s a habit you’d like to better control.
It’s always wise to check with your doctor — she should be able to help you decide whether it is best for you to cut back or to abstain. People who are dependent on alcohol, or have other medical or mental health problems, should stop drinking completely.
But many people may benefit simply by cutting back. If your doctor suggests that you curb your drinking, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) suggests that the following steps may be helpful:

https://x.com/i/broadcasts/1ynKOlrpYWWGR

World Health Day, celebrated on 7 April 2025, will kick off a year-long campaign on maternal and newborn health. The campaign, titled Healthy beginnings, hopeful futures, will urge governments and the health community to ramp up efforts to end preventable maternal and newborn deaths, and to prioritize women’s longer-term health and well-being.
WHO and partners will also share useful information to support healthy pregnancies and births, and better postnatal health.
Visit the World Health Day 2025 campaign page
This task is critical. Tragically, based on currently published estimates, close to 300 000 women lose their life due to pregnancy or childbirth each year, while over 2 million babies die in their first month of life and around 2 million more are stillborn. That’s roughly 1 preventable death every 7 seconds.
Based on current trends, a staggering 4 out of 5 countries are off track to meet targets for improving maternal survival by 2030. 1 in 3 will fail to meet targets for reducing newborn deaths.
Women and families everywhere need high quality care that supports them physically and emotionally, before, during and after birth.
Health systems must evolve to manage the many health issues that impact maternal and newborn health. These not only include direct obstetric complications but also mental health conditions, noncommunicable diseases and family planning.
Additionally, women and families should be supported by laws and policies that safeguard their health and rights.
Here’s what you can do to support the campaign:



·
As more people are drinking less, there’s been an uptick in more drink companies creating nonalcoholic options. But it can still be tough to figure out which of these options are healthy. Keep an eye on ingredients like sugar, artificial sweeteners and caffeine. If you’re choosing nonalcoholic alternatives, consider options that are low in added sugars and free from unnecessary additives. Consulting a healthcare provider can help ensure your choices support your overall well-being.
Show more

Why the idea that “a little red wine is good for your heart” doesn’t hold up anymore.
I used to drink.
A lot more than I should have.
And while I had some seriously good times when I was drinking, it came at a huge cost.
Brutal hangovers. Terrible sleep. Wrecked weekends.
Even a broken back.
(But that’s a story for another day.)
I still drink.
But just very little these days.
As a cardiologist, I am asked almost every day if ‘Alcohol is good or bad for your health?’.
Let’s find out.
There is no getting away from the fact that, at its most basic chemical foundation, alcohol is a toxin.
Globally, alcohol is responsible for 3 million deaths per year; in the United States, it is the third leading cause of preventable death¹².
Alcohol is a factor in³:
Alcohol is a factor in 1 in 5 emergency department presentations⁴.
No pun intended, but these statistics make for some sober reading.
‘Red Wine Is Good For Your Heart.’
Now come on.
Did you really think that was true?
I have heard this phrase over and over again in my clinical practice.
High levels of exercise are good for your heart, but oddly enough, most people seem to be far less enthusiastic about this approach than regular alcohol consumption.
Let’s see what the data says.
Up until very recently, it was believed that drinking 1-2 drinks per day was actually protective when it came to dying prematurely⁵.

This data was based on observational studies that cannot fully control for all confounders and can therefore not infer causality.
When you examine the people who drink only 1 to 2 drinks per day, you consistently find that they are much less likely to smoke, be overweight or engage in any other risky health behaviours.
So in truth, it probably wasn’t the alcohol that was driving the effect.
More recent studies have attempted to control for this variable more carefully, and the relationship is clear.
The more you drink.
The higher the risk.
Take coronary artery disease. Higher alcohol intake equates to a higher risk.
The same applies to high blood pressure⁶.

The same applies to stroke⁷.
The list goes on⁸:
You get the point.
With all this information to hand, why is it then that I and billions of others continue to drink alcohol?…
Become a paying subscriber of Dr Paddy Barrett to get access to this post and other subscriber-only content.
| Subscriber Only Posts & Access To Full Archive | |
| 25% Discount On Live Education Sessions & AMA’s | |
| Discounts On Courses & Live Education Sessions & AMA’s |

·
A baby who can self-soothe will fall asleep on their own and play calmly without your intervention. It’s a process, and a skill, that will help throughout their lives. Follow these tips to get started.
It’s naptime — thank goodness. But your baby isn’t having it. They cry. They fuss. So, you bounce them, rock them or even drive around town until they fall asleep.
It’s the question on the top of your mind (and you’re not alone): When — and how — will my baby learn to self-soothe and calm down without so much effort?
Pediatrician Matthew Badgett, MD, answers this important question, and shares ways to help your baby learn to self-soothe.
When your baby self-soothes, they can calm down on their own and they:
But self-soothing isn’t just for little ones. It’s an important skill throughout your life. Whether you realize it or not, you use your own self-soothing methods to feel better when you’re stressed or anxious.
“Self-soothing is a way of regulating your emotions,” Dr. Badgett explains. “Babies might suck their thumb or hold a stuffed animal. Adults might listen to music, take a walk or do yoga. The type of self-soothing you use changes throughout your life, but it’s a key part of your emotional health.”
Every exhausted parent wants to know: When will my baby lie in their crib and drift off to sleep without my help? Or When can I put them in their bouncy seat for five minutes without screams of protest?
“In general, don’t try to teach your baby to self-soothe before they are 3 months old,” advises Dr. Badgett. “Newborns need you to help soothe them because they don’t have the ability to control their emotions. Learning emotional control is a process that takes years, so don’t expect too much from an infant or toddler.”
And self-soothing is a gradual process — not a switch you can flip. “Self-soothing is really co-soothing because the parent is still involved,” says Dr. Badgett. “Your baby plays a more active role in soothing, but you set them up for success. You figure out how your baby can calm down with less of your help.”
If your baby is past the newborn stage but still cries relentlessly when you put them down, there is hope. These tips can help your baby gain self-soothing skills:
Before you assume that your baby is just cranky, review their list of needs. Your baby won’t be able to self-soothe if:
After you’ve ruled out those issues, move on to the next steps.
Babies love routine. Try to put your baby to bed at the same time every day. Don’t skip naps or keep your baby up late. A schedule keeps them from becoming overtired — that’s when any hope of self-soothing goes out the window.
“If your baby goes to bed at the same times each day, their body clock will get used to it,” Dr. Badgett notes. “Then, they will start to feel sleepy right at naptime or bedtime. Babies that are drowsy, but not exhausted, are better able to fall asleep on their own.”
The sound of a fan or a white noise machine can be music to your baby’s ears. “Many babies prefer a steady sound over a perfectly quiet room,” Dr. Badgett says. “It helps drown out other sounds that could startle them, and it has a calming effect.”
Turn on the white noise machine when it’s bedtime. This can serve as a cue for your baby to learn when it’s time for dreamland.
After you place your baby in their crib or seat, don’t leave right away.
“If you give your baby some attention without holding them, they learn that being put down isn’t a bad thing,” Dr. Badgett explains. “Talk to them, or gently put your hand on their belly. After a few minutes, calmly leave the room.”
Pacifiers are a useful tool for babies under the age of 1. But use caution. It can be hard to take the paci away from a baby who can’t calm down without it.
“Pacifiers help young babies learn to self-soothe before they learn other techniques,” Dr. Badgett says. “But limit pacifier use to naptime and bedtime. Use them with other methods, like white noise and a consistent routine. That way, your baby won’t learn to rely on the pacifier alone.”
It’s normal for young babies to fall asleep at the bottle or breast. But as your baby grows, they need to learn other ways to drift off.
“Don’t feed your older baby right at naptime with the sole purpose of getting them to sleep,” Dr. Badgett suggests. “They might end up overeating or relying on the nipple even when they’re already full.”
You can avoid the feed-to-sleep method if you:
With a little persistence, perseverance and patience on your end, your little one could be self-soothing to sleep in no time.