If you run regularly, whether it’s an easy jog around the block to stay fit or an intense training regimen to prepare for a marathon, you need proper nutrition.
Here are some tips to help keep runners well-nourished and ready to win.
Foods for Runners and Joggers
A good diet can boost your physical health and help you meet your fitness goals. Make sure your meals emphasize the following basic components:
- Fruit and vegetables for vitamins, minerals and antioxidants
- Lean protein such as fish, poultry, beans, lentils and tofu
- Healthy fats such as olive oil, avocado and nuts
- Healthy carbohydrates such as rice, whole grain breads/pastas and oatmeal
Individuals may have different optimal balances, but in general, people who include running or jogging as part of their fitness regimen should get 60% to 70% of their calories from carbohydrates, with lean protein and healthy fats each accounting for 15% to 20% of their remaining calories.
Don’t skimp on carbohydrates
Although low carbohydrate diets are popular go-to’s for people wanting to lose weight, they’re not ideal for distance runners, who thrive on carbohydrates for endurance.
That is why very low carbohydrate diets, such as the ketogenic diet, plus running is not a good idea. Experts do not recommend keto to runners unless they have been told by their doctor that this a medically safe option for them and they are being monitored while in ketosis.
Distance runners need more carbs than people who aren’t training. Undereating carbohydrates can be hard on your body and affect your recovery after your run.
Here’s why: Running uses both glucose in the blood and your stores of glycogen. Glucose is the form of sugar that circulates in the bloodstream, and glycogen is the sugar stored in your liver and muscles that acts as the primary fuel for endurance exercise.
Eating plenty of carbs helps ensure that these energy stores are ready to support your training. When those stores get too low, runners are more likely to run out of energy and “burn out” or “hit a wall” while training.
Running Diet — Vitamins and Minerals
Running changes your body and your nutritional needs. Often when people start a running regimen, they are trying to lose weight or get in shape quickly, and they don’t realize they need to adjust their diet.
Especially in women runners, dietitians report seeing a tendency to overdo the running while not eating enough, and this can have an effect on health if they do not adequately replenish lost vitamins and minerals in their diet.
For women in particular, calcium and vitamin D are essential for bone health to avoid loss of bone mineral density and the risk of stress fractures.
For more vitamin D, include these foods in your meals:
- Vitamin D-fortified dairy and almond, soy or rice based beverages
- Eggs
- Cereal fortified with vitamin D
- Tuna
- Salmon
For more calcium, try:
- Yogurt and cheese
- Tofu
- Edamame
- Almonds
- Canned fish with bones (such as sardines)
Iron deficiency can affect women and even have an impact on their running performance. Menstruation puts people at higher risk of iron deficiency, and if iron isn’t replenished in the diet, decreases in hemoglobin can occur and bring on anemia. Hemoglobin is what carries oxygen throughout the body, including the muscles, so if there is a deficit, the muscles may feel the effect of insufficient oxygen during exercise.
Iron-rich foods include:
- Poultry and other meat
- Legumes, such as peas and beans
- Dark, leafy green vegetables such as kale
- Dried fruits and raisins
- Iron-fortified breads and cereals
Dietitians recommend eating eating iron rich foods in combination with foods high in vitamin C, such as citrus, bell peppers or berries, since vitamin C helps increase the body’s absorption of iron.
What to Eat Before Running ― and When
The best time to eat a full meal is about two to three hours before you hit the road, track or trail. Have a good source of carbs paired with protein, making sure the meal focuses on a healthy carb source.
If it’s been more than three to four hours since you’ve eaten, a carbohydrate-rich snack a half-hour before running can ensure you have adequate glucose available before you head out. Directly before a run, it’s best to stick with easy-to-digest carbohydrates to avoid gastrointestinal [GI] distress such as cramping or diarrhea.
Try these:
- Bananas
- Applesauce
- Crackers, pretzels or cereal
- White bread
- Potatoes
Glucose Boosters for Long Distance Runners
If you are training for a marathon or distance event and are going to be out for over an hour, you will want to bring some fuel with you. Energy drinks, gel tubes and other sources of quick blood-glucose boosters are available, but you can also use something as simple as fruit snacks.
Try practicing with these items as you train so you can pick the formulas that are best for you, and you can work on accessing and ingesting them smoothly without breaking stride.
What foods should runners avoid?
Before a run or the night before a big race, Eidel recommends going easy on:
- Spicy foods or foods overly high in fat, which can cause GI upset
- Foods that are very high in fiber, which can cause gas and cramping
- Caffeine ― Although it is tempting to grab a caffeine boost right before a run, runners should remember that for some people, caffeine can stimulate the GI tract, which can result in diarrhea or the need for an emergency bathroom break
Does carb-loading work?
It might. Carb loading is the practice of eating a lot of carbohydrates ― particularly those that are easily absorbed, such as white bread, pasta and rice ― for 24 to 48 hours before a big race or distance run, to shore up your body’s stores of glycogen and lessen the risk of burnout before finishing the event.
Some studies show carb loading is beneficial for people preparing for a race, but it’s important to make sure during that time you’re also allowing your body to rest and giving it time to store what you are ingesting. The number of carbohydrate grams will be differ from person to person, but in general, evidence shows carb loading can be beneficial prior to a distance event.
In contrast, casual runners likely do not need to carb load. Ensuring that their day-to-day diets include extra carbohydrates can be sufficient.
What to Eat After a Run
It’s common for people not to feel hungry after a run, but a snack or light meal of complex carbohydrates and protein within the first hour after running can help replenish glycogen stores and to support recovery and rebuild stressed muscles. For example:
- Peanut butter and banana
- Egg on toast
- Sandwich with deli meat
- Pasta with meat or plant-based protein
- Veggie burger on a bun
- Protein shake or smoothie
Running to Lose Weight
If you’re interested in running as part of a weight loss plan, getting adequate nutrition is a must. Even casual running or jogging burns calories and can be hard on the body. Runners can become undernourished at first because they don’t understand how much energy they’re burning when they run and what they need to properly recover.
Eating enough is also essential to building muscles, which can aid in fat burning ― a plus for people working on achieving or maintaining a healthy weight.
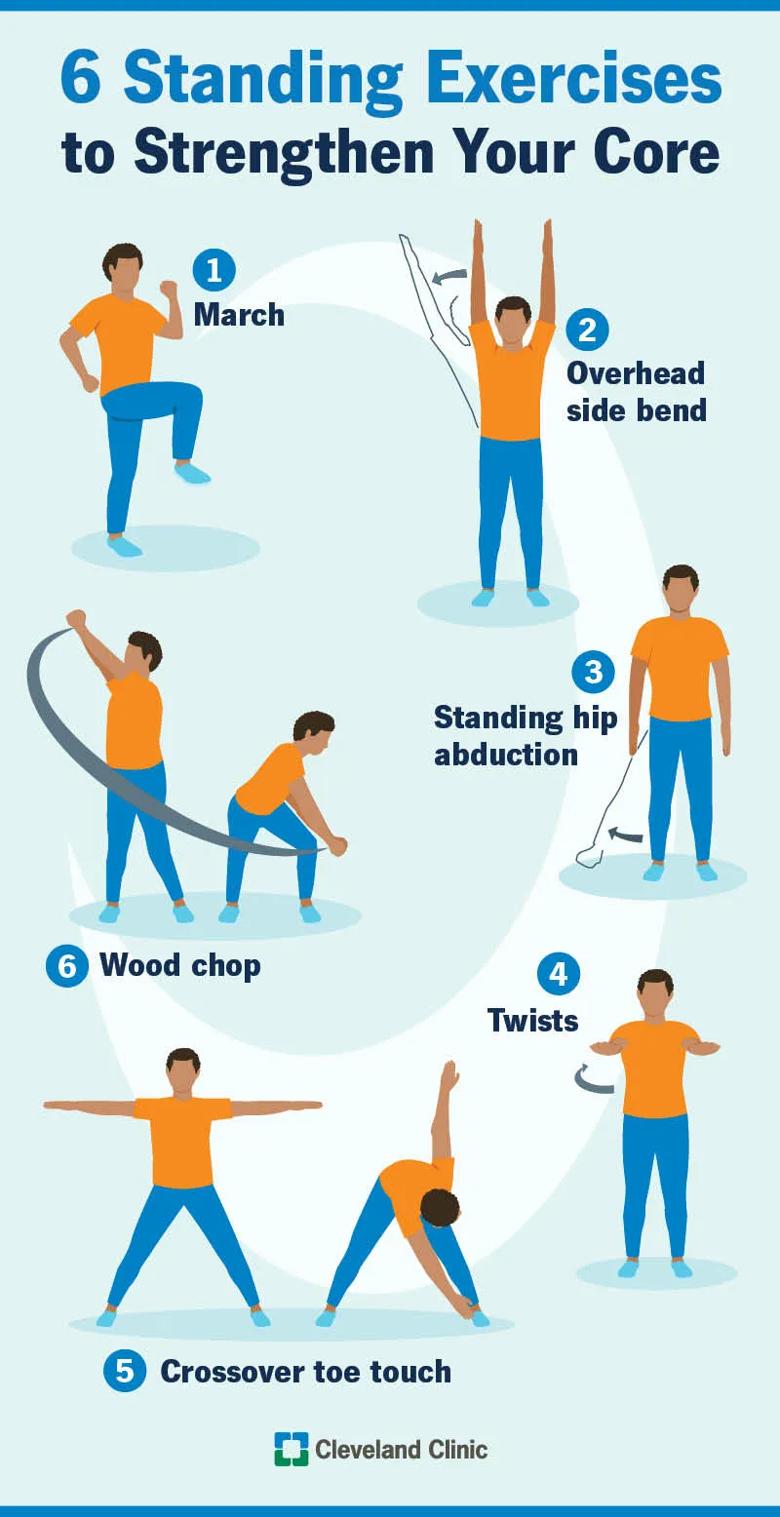
For optimal weight loss, your plan should not rely on running alone but also include strength training and proper nutrition.
Listen to your body
If you run regularly, you should pay attention to the effects of what you eat and when, especially on running performance. Learning what works best for you can take some time and a little trial and error, but it is worth it, since running, jogging and other regular aerobic exercise offers so many health advantages.
Always feel free to consult a dietitian or doctor, and listen to your body if you’re not keeping up with your training goals.